Search
- Page Path
- HOME > Search
- Clinical Study
- Association between Secondhand Smoke Exposure and Metabolic Syndrome in 118,609 Korean Never Smokers Verified by Self-Reported Questionnaire and Urine Cotinine
- Ji Hye Kim, Byung Jin Kim, Young Youl Hyun, Jin Ho Kang
- Endocrinol Metab. 2020;35(4):892-900. Published online December 23, 2020
- DOI: https://doi.org/10.3803/EnM.2020.847
- 4,286 View
- 100 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
No study has reported the association between secondhand smoke (SHS) exposure and metabolic syndrome (MetS) in self-reported never smokers verified by both self-reported questionnaire and urine cotinine.
Methods
A total of 118,609 self-reported and cotinine-verified never smokers (38,385 male; age 34.8±7.1 years) who participated in the Kangbuk Samsung Health Study between 2011 and 2016 were included. Cotinine-verified never smokers were defined as individuals with urinary cotinine <50 ng/mL. SHS exposure was defined as current exposure to passive smoking indoors at home or workplace.
Results
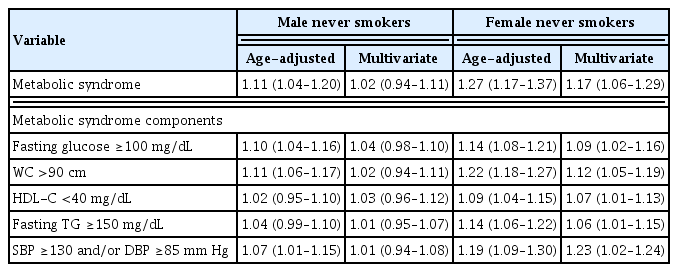
Prevalence of SHS exposure in the overall population was 22.6% (27.4% for males and 20.3% for females (P<0.001). The overall prevalence of MetS was 6.8% and was higher in males than in females (10.7% vs. 4.9%, P<0.001). In both genders, MetS prevalence was higher in the SHS exposure group than the non-SHS exposure group (11.3% vs. 10.4%, P=0.010 for males; 5.8% vs. 4.6%, P<0.001 for females). However, there was significant gender interaction for the association between SHS exposure and MetS (P for interaction=0.010). In the multivariate regression analyses, SHS exposure was associated with increased MetS odds only in females (odds ratio [95% confidence interval], 1.02 [0.94 to 1.11] in male vs. 1.17 [1.06 to 1.29] in female). In particular, females with SHS exposure of ≥1 hour/day and ≥3 times showed increased odds of MetS compared with those without SHS exposure (1.22 [1.02 to 1.45], 1.30 [1.14 to 1.49]).
Conclusion
This cross-sectional study showed that SHS exposure was significantly associated with prevalence of MetS in self-reported and cotinine-verified female never smokers. -
Citations
Citations to this article as recorded by- Combined Influence of Eight Lifestyle Factors on Metabolic Syndrome Incidence: A Prospective Cohort Study from the MECH-HK Study
Yun-Yang Deng, Fei-Wan Ngai, Jing Qin, Lin Yang, Ka-Po Wong, Harry-Haoxiang Wang, Yao-Jie Xie
Nutrients.2024; 16(4): 547. CrossRef - Association of Zinc Intake, Tobacco Smoke Exposure, With Metabolic Syndrome: Evidence from NHANES 2007–2018
Shengxiang Yang, Qian Chen, Lin Wang
Biological Trace Element Research.2024;[Epub] CrossRef - The association between urinary cotinine level and metabolic syndrome profiles among adolescents: findings from the Ewha Birth and growth study
Hyunjin Park, Ui-Jeong Kim, Eun Jeong Choi, Seunghee Jun, Bomi Park, Hye Ah Lee, Hae Soon Kim, Hyesook Park
BMC Public Health.2023;[Epub] CrossRef - Association of environmental tobacco smoke exposure with metabolic syndrome: A longitudinal Cohort Study of 71,055 never smokers
Hyo-In Choi, Seung Jae Lee, Jeong Gyu Kang, Sung Ho Lee, Bum Soo Kim, Byung Jin Kim
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(11): 2534. CrossRef
- Combined Influence of Eight Lifestyle Factors on Metabolic Syndrome Incidence: A Prospective Cohort Study from the MECH-HK Study

- Clinical Study
- Eligibility for Statin Treatment in Korean Subjects with Reduced Renal Function: An Observational Study
- Byung Sub Moon, Jongho Kim, Ji Hyun Kim, Young Youl Hyun, Se Eun Park, Hyung-Geun Oh, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Kyu-Beck Lee, Hyang Kim, Sung-Woo Park, Eun-Jung Rhee
- Endocrinol Metab. 2016;31(3):402-409. Published online August 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.402
- 3,955 View
- 33 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study was to investigate the relationship between statin eligibility and the degree of renal dysfunction using the Adult Treatment Panel (ATP) III and the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines in Korean adults.
Methods Renal function was assessed in 18,746 participants of the Kangbuk Samsung Health Study from January 2011 to December 2012. Subjects were divided into three groups according to estimated glomerular filtration rate (eGFR): stage 1, eGFR ≥90 mL/min/1.73 m2; stage 2, eGFR 60 to 89 mL/min/1.73 m2; and stages 3 to 5, eGFR <60 mL/min/1.73 m2. Statin eligibility in these groups was determined using the ATP III and ACC/AHA guidelines, and the risk for 10-year atherosclerotic cardiovascular disease (ASCVD) was calculated using the Framingham Risk Score (FRS) and Pooled Cohort Equation (PCE).
Results There were 3,546 (18.9%) and 4,048 (21.5%) statin-eligible subjects according to ATP III and ACC/AHA guidelines, respectively. The proportion of statin-eligible subjects increased as renal function deteriorated. Statin eligibility by the ACC/AHA guidelines showed better agreement with the Kidney Disease Improving Global Outcomes (KDIGO) recommendations compared to the ATP III guidelines in subjects with stage 3 to 5 chronic kidney disease (CKD) (κ value, 0.689 vs. 0.531). When the 10-year ASCVD risk was assessed using the FRS and PCE, the mean risk calculated by both equations significantly increased as renal function declined.
Conclusions The proportion of statin-eligible subjects significantly increased according to worsening renal function in this Korean cohort. ACC/AHA guideline showed better agreement for statin eligibility with that recommended by KDIGO guideline compared to ATP III in subjects with CKD.
-
Citations
Citations to this article as recorded by- Association between atherosclerotic cardiovascular diseases risk and renal outcome in patients with type 2 diabetes mellitus
Honghong Ren, Lijun Zhao, Yutong Zou, Yiting Wang, Junlin Zhang, Yucheng Wu, Rui Zhang, Tingli Wang, Jiali Wang, Yitao Zhu, Ruikun Guo, Huan Xu, Lin Li, Mark E. Cooper, Fang Liu
Renal Failure.2021; 43(1): 477. CrossRef - Long-term effects of various types of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on changes in glomerular filtration rate in Korea
Seo Yeon Baik, Hyunah Kim, So Jung Yang, Tong Min Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
Frontiers of Medicine.2019; 13(6): 713. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef
- Association between atherosclerotic cardiovascular diseases risk and renal outcome in patients with type 2 diabetes mellitus


 KES
KES

 First
First Prev
Prev



